Breast Engorgement Relief: A Guide to Managing Pain and Swelling
Breast engorgement is a common, and often uncomfortable, part of early breastfeeding. As a lactation consultant, I see many new parents worry that engorgement means something is wrong with their milk supply or latch. The good news is that engorgement is usually temporary and very manageable with the right support.
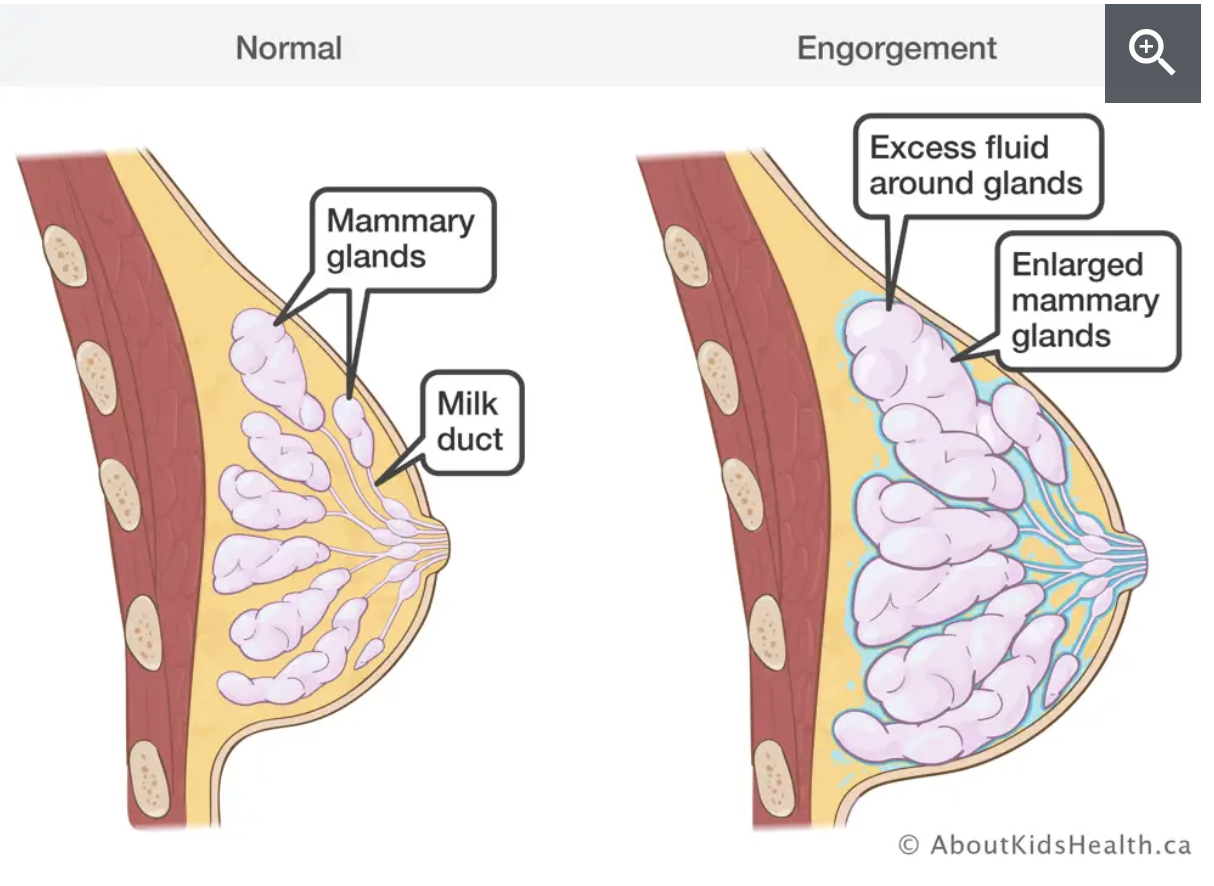
Engorgement happens when milk supply increases and fluid builds up in the breast tissue. Effective engorgement management focuses on reducing swelling while allowing milk to flow, so your baby can feed comfortably and your body can regulate supply.
What Causes Breast Engorgement?
Engorgement most often occurs:
In the first few days postpartum as milk “comes in”
When feedings are delayed or skipped
If milk removal is less effective (poor latch, sleepy baby, separation)
Breasts may feel firm, heavy, warm, or painful, and nipples can become flattened, making latching harder.
Engorgement Management Tips
1. Reduce Swelling Before Nursing
Before feeding, apply a cold compress or ice pack to the breasts for about 5-10 minutes. Cold helps reduce inflammation and tissue swelling, making it easier for milk to flow. If you had a swollen ankle, you would also ice it!
You may also use ibuprofen for inflammation, as recommended by your healthcare provider.
2. Use “Breast Gymnastics” & Therapeutic Breast Massage
Before feeding or pumping, use gentle breast movement to help shift excess fluid away from the milk ducts, so milk can flow more easily.
Therapeutic breast massage (see the video here)
Light, gentle stroking of the breast toward the armpit
Avoid deep or forceful massage, which can worsen swelling
Think of the firmness of petting a cat or dog
Breast gymnastics (pioneered by Maya Bolman, and seen in the video below)
Lift the breast
Move it side to side
Move it up and down
Gently circle the breast
3. Soften the Areola to Improve Latch
If the areola feels firm or tight, your baby may struggle to latch deeply.
Reverse Pressure Softening (RPS) can help, especially in the early days when swelling is strongest:
Uses gentle fingertip pressure around the nipple
Temporarily moves fluid away from the areola
Makes the breast softer and easier to latch
Step-by-step guide is here and images are from WIC Arizona.
4. Nurse/Pump as Often As Your Baby Shows Hunger Cues
Frequent milk removal is key.
Aim for at least 8–10 feeds in 24 hours if your baby is a newborn
Follow your baby’s feeding cues
If your baby is sleepy or feeds are short, an IBCLC can help assess milk transfer and latch.
5. Express Milk for Comfort
If breasts still feel overly full after feeding:
Hand express or pump just enough for comfort
Avoid fully emptying unless advised, as over-pumping can worsen engorgement by signaling increased supply
The goal is relief, not extra stimulation.
How Long Does Engorgement Last?
With consistent management, engorgement usually improves within 24–48 hours. If swelling, pain, or redness worsen, or if you develop fever or flu-like symptoms, reach out to a lactation consultant or healthcare provider promptly.
When to Seek Breastfeeding Help From an IBCLC
If engorgement:
Persists beyond a couple of days
Makes latching difficult
Leads to nipple pain, plugged ducts, or mastitis
Is paired with concerns about milk supply or baby’s intake
Professional breastfeeding help from an IBCLC can make a significant difference, especially in the early postpartum period when your milk supply is regulating.
Engorgement can feel intense, but it is usually a short-lived phase. With gentle techniques, frequent feeding, and personalized guidance, most parents find relief quickly and go on to have a more comfortable breastfeeding experience.
If you’re pregnant and want to plan ahead, or postpartum and struggling right now, lactation support is available.
If you’re experiencing breast engorgement or want personalized breastfeeding support, consider scheduling a lactation consultation with an IBCLC for prenatal or postpartum care.
Written by Kathleen Stern (bio here). For more infant feeding and parent support, reach out to Kathleen at www.strongnestconsulting.com
Last updated December 19, 2025